Your period doesn’t behave the same way every month, and most of the time, hormones are the reason. A small shift in estrogen or progesterone can change your flow from light to heavy, make cramps stronger, affect your skin, or even cause irritation that makes certain pads uncomfortable. Many people experience these changes but never fully understand why their flow reacts this way. This guide breaks down how hormones shape your menstrual cycle, how they influence the type of sanitary towels you may need, and how to respond to those changes so you stay comfortable and protected. You’ll also learn what causes hormonal shifts and simple steps that may help keep your cycle steady.
The Hormones Behind Your Menstrual Cycle
Estrogen’s Role in Regulating Flow & Cycle Length
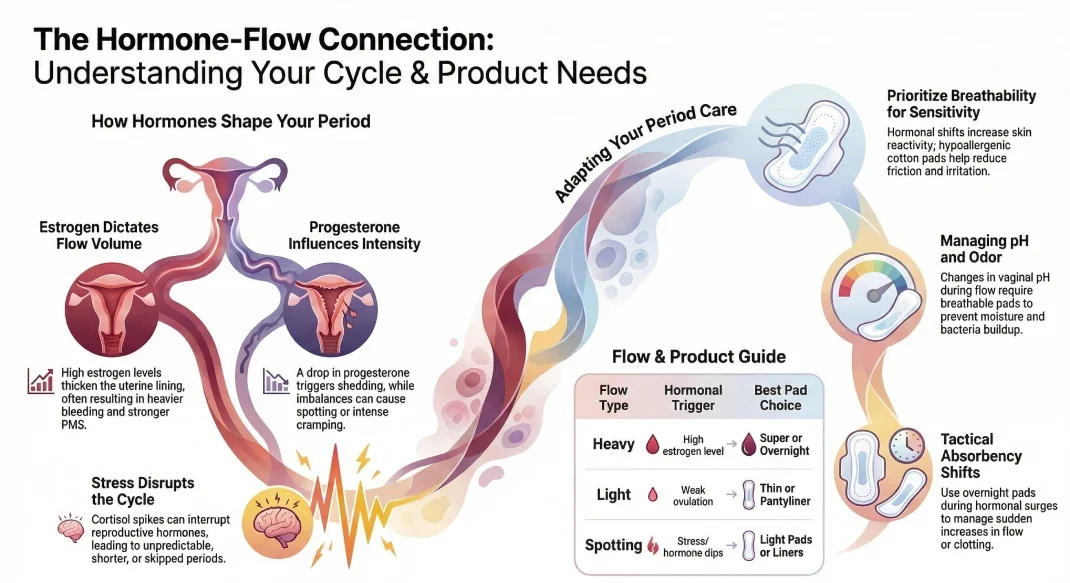
Estrogen helps thicken the uterine lining and also supports stable cycle timing. When estrogen stays balanced, your period usually follows a predictable pattern. Low estrogen may lead to lighter flow or skipped cycles, while high estrogen can cause heavier bleeding and stronger PMS. People often notice breast tenderness and mood changes when estrogen levels swing too fast.
How Progesterone Affects PMS, Cramps, and Flow Intensity
Progesterone rises after ovulation and gets your body ready for a possible pregnancy. If pregnancy doesn’t happen, the drop in progesterone causes the lining to shed, your period. Low progesterone may lead to spotting or short cycles, while high progesterone can cause bloating, fatigue, and emotional ups and downs. This hormone also influences how strong your cramps feel because it interacts with prostaglandins.
Other Hormones That Influence Your Cycle
FSH and LH help your ovaries release an egg each month. If these hormones shift, ovulation may be delayed or may not occur at all, which often results in irregular bleeding. Prostaglandins control uterine contractions and can affect cramping and clotting. High prostaglandin levels are one of the most common reasons for painful periods.
What “Hormonal Imbalance” Means for Your Period
A hormonal imbalance doesn’t always mean something serious. It simply means the hormones guiding your cycle aren’t working in sync. This can lead to unpredictable flow, stronger PMS, breakouts, mood swings, or changes in pad absorbency needs. Understanding this helps you choose the right period products and recognize when your body needs extra support.
What Causes Hormonal Changes That Affect Period Flow?
Many things in daily life impact hormone levels, from stress and diet to medical conditions. When these factors shift your hormones, your flow may change in color, thickness, timing, or heaviness. Recognizing these triggers can help you adjust your sanitary towel choices and your daily routine.
Lifestyle Factors: Stress, Sleep Loss & Cortisol Spikes
Stress pushes your body to release cortisol, which can interrupt estrogen and progesterone. When cortisol stays high, cycles may become shorter, longer, or unpredictable. Poor sleep can also raise cortisol, which explains why many people experience unusual cycles during stressful periods of life.
Thyroid Disorders
Your thyroid helps regulate metabolism, energy, and hormone production. Low thyroid activity (hypothyroidism) may cause heavy bleeding and fatigue, while high thyroid activity (hyperthyroidism) may cause lighter or irregular periods. Many people with thyroid issues also notice changes in skin sensitivity, which can affect how pads feel against the skin.
PCOS & Insulin Resistance
Polycystic Ovary Syndrome disrupts normal ovulation, leading to irregular cycles, heavier flow, acne, and hair changes. Insulin resistance often comes with PCOS and influences hormone production. People with PCOS may need different pad absorbencies depending on whether their flow is light, heavy, or unpredictable.
Birth Control, Emergency Contraceptives & Medication Side Effects
Birth control adjusts hormone levels to prevent pregnancy, but it can also change flow patterns. Some people see lighter periods, while others may notice breakthrough bleeding. Emergency contraceptives may cause a heavier or delayed period due to sudden hormone changes. Certain medications, such as antidepressants or steroids, can also shift hormone activity.
Nutrient Deficiencies That Affect Hormones
Your body needs key nutrients to keep hormones steady. Low iron can lead to fatigue and worsen heavy bleeding, while low vitamin D or B vitamins may disrupt cycle regularity. Omega-3 fatty acids help support inflammation control and may reduce severe PMS when levels are adequate.
Age-Related Hormonal Shifts
Teenagers often experience irregular cycles as their hormones settle. People in their 30s and 40s may notice changes due to natural shifts in estrogen and progesterone. Perimenopause can cause heavy or light flow, skipped periods, or sudden month-to-month changes.
How Hormonal Shifts Show Up in Your Period Symptoms
Hormones influence almost every change you notice during your cycle. When they rise too high or dip too low, your body reacts in ways that affect your period’s timing, texture, color, and overall comfort. Many people experience these symptoms without realizing they are tied directly to estrogen, progesterone, thyroid hormones, or prostaglandins. Understanding these signs makes it easier to adjust your sanitary towel choice and keep track of your body’s patterns month after month.
Irregular or Missed Periods
When hormones are out of sync, ovulation may not occur on time or at all. This often results in cycles that arrive earlier, later, or skip a month entirely.
Sudden Changes in Color, Odor, or Clotting
Hormones can influence how quickly the lining sheds, which affects color and thickness. High prostaglandins may create thicker clots, while slow shedding may result in darker blood. Odor shifts sometimes occur when hormones affect vaginal pH. These changes are common, but monitoring them helps you catch unusual patterns early.
Mood Swings, PMS, and PMDD
Emotional changes are often the first sign of shifting hormones. A rise in progesterone may lead to sadness, irritability, and fatigue. A sharp drop in estrogen may trigger crying spells or tension. People with PMDD feel these symptoms more strongly. These emotional shifts can make physical comfort more important, including choosing softer, breathable pads.
Skin Breakouts, Hair Changes, and Water Retention
When estrogen and progesterone fluctuate, oil production can increase, leading to acne. Some people see thinning hair or more shedding when hormonal changes are more intense. Water retention can cause bloating and pressure around the stomach and thighs. These symptoms may also make tight clothing uncomfortable, increasing the need for pads that sit smoothly and feel gentle on the skin.
How Hormones Influence Your Sanitary Towel Needs
Hormonal changes affect flow levels, skin sensitivity, and comfort needs. This is why the same pad doesn’t work for every phase of your cycle. Some days you may need high absorbency for heavy bleeding, while other days call for a thinner, breathable option. Understanding this variation helps you stay prepared and protected, especially when your cycle can shift unexpectedly.
Choosing Pad Absorbency Based on Flow Changes
| Flow Type | Hormonal Trigger | Best Pad Choice |
| Heavy | High estrogen | Super or overnight absorbency |
| Moderate | Balanced cycle | Regular pads |
| Light | Weak ovulation or low progesterone | Thin or pantyliner pads |
| Spotting | Hormone dips or stress | Light pads or liners |
How Hormonal Breakouts & Sensitivity Affect Pad Material Choice
Hormones can make your skin more reactive, which means pads with rough textures or synthetic materials may cause itching or irritation. Many people prefer cotton or hypoallergenic pads during sensitive days because they reduce friction and feel calmer against inflamed skin.
Comfort Needs During PMS: Cushioning, Softness & Breathability
PMS bloating and cramps may make your lower abdomen tender. Soft, cushioned pads feel more comfortable and can ease pressure during this time. Breathability also helps reduce heat buildup, which can worsen irritation when hormones make the skin reactive.
Managing Heavy Flow Triggered by Hormonal Surges
During months when hormones cause a thicker lining, your period may release more blood in a shorter time. High-absorbency pads help prevent leaks and allow you to move freely. Overnight pads are useful even during the day if your flow increases suddenly.
Preventing Odor & Bacteria Growth When Hormones Shift pH Levels
Hormonal fluctuations affect vaginal pH, which can make odor more noticeable. Breathable pads help reduce moisture, while pads with neutral pH layers help maintain freshness. Avoiding plastic-heavy pads can also reduce heat and sweat buildup.
Natural Ways to Support Hormonal Balance
Hormonal changes can affect flow, mood, energy, and even the type of pads you need each month. While medical treatment is essential for certain conditions, simple habits can support your body and help keep your cycle steady. These approaches don’t replace medical care, but they give your hormones a healthier environment to work in. Many people notice improvements in PMS, flow patterns, and daily comfort when they build these habits into their routine.
Nutrition for Hormone Health
Food plays a major role in shaping how your hormones behave each month. Your body depends on nutrients from meals to support estrogen, progesterone, and insulin, which all influence your period flow and PMS symptoms. When you eat balanced meals rich in fiber, whole grains, healthy fats, and natural protein sources, your hormones have what they need to stay steady. Fruits and vegetables help control inflammation, whole grains support blood sugar balance, and healthy fats assist in hormone production.
Foods rich in omega-3s, like salmon or chia seeds, support cycle regularity and may reduce cramps. Iron-rich foods such as beans, spinach, and lean meats help your body recover from monthly blood loss. Reducing processed foods and sugary snacks may also help because these can trigger insulin spikes that affect ovarian hormones. Staying hydrated keeps your blood circulating properly and may ease bloating during PMS.
Exercise That Supports Hormone Stability
Regular movement helps your body control insulin, lower cortisol, and support reproductive hormones. Exercise improves blood flow, reduces cramps, and helps ease stress-related PMS symptoms. Gentle stretching or yoga can relax tight muscles, while strength training supports your metabolism and keeps your body strong as hormone levels shift through the month. Walking or light cardio helps reduce bloating and boosts energy on days when you feel sluggish. Short home workouts can also make a difference when done consistently. Many people find that even 20 to 30 minutes of activity each day helps bring more predictable cycles and reduces the intensity of PMS.
Sleep Habits That Help Hormones Stay Steady
Your body depends on sleep to reset hormone levels. When sleep is interrupted or too short, cortisol rises and interferes with the hormones that guide your menstrual cycle. A steady sleep routine helps estrogen and progesterone remain balanced and can lead to more predictable flow patterns. Going to bed at the same time each night helps regulate your internal clock. A dark, cool room can improve sleep quality, and reducing screen use before bed helps your brain wind down. Avoiding caffeine late in the day also supports deeper rest. Consistent sleep is especially helpful for people who see heavier or lighter bleeding during stressful weeks.
Stress Management Techniques
High stress pushes your body into a state that makes hormone control more difficult. This often leads to irregular cycles, heavier bleeding, and stronger PMS symptoms. Building simple stress relief habits into your day can make a big difference. Deep breathing exercises calm your nervous system and lower cortisol. Gentle stretching before bed helps your muscles relax, while short outdoor walks can reset your mood and clear your mind. Talking to someone you trust may ease emotional pressure, and taking mindful breaks during busy work hours can prevent stress from piling up. Keeping stress levels lower often brings better flow consistency and less discomfort throughout your cycle.
When Hormone-Related Period Changes Require Medical Attention
Most hormonal shifts are normal, but some changes need a doctor’s evaluation. If your flow becomes unusually heavy, extremely painful, or unpredictable for several months, it may point to a deeper issue such as PCOS, thyroid problems, fibroids, or long-term hormone disruption. Getting medical help early prevents symptoms from getting worse and ensures you have the right treatment plan. Understanding how hormones work helps you choose the right sanitary towel for comfort, absorbency, and skin health
Warning Signs of a Serious Hormone Problem
Some symptoms suggest that hormone levels are moving far outside their usual range and need evaluation. Periods that come more than 45 days apart may indicate problems with ovulation. Bleeding that lasts longer than a week or becomes heavy enough to require pad changes every one to two hours may signal issues with estrogen or the uterine lining. Pelvic pain that feels sharp or constant, sudden acne flare-ups, unusual hair changes, or unexpected weight gain or loss can also point to a hormone imbalance. These symptoms should not be ignored, especially if they appear repeatedly.
Diagnostic Tests Doctors Use
Doctors use several methods to understand what is causing hormonal changes. Blood tests can measure estrogen, progesterone, thyroid hormones, and insulin levels. Thyroid tests are especially important because thyroid imbalance affects cycle timing and flow. Ultrasound scans help check the ovaries and uterus for cysts, fibroids, or lining thickness. Iron studies reveal whether heavy bleeding has caused anemia. These tests give a clearer picture of whether the cause is hormonal or related to a structural issue inside the reproductive system.
Treatments You May Be Offered
Treatment depends on the cause of your symptoms. Doctors may recommend medications that help balance hormone levels or suggest birth control pills or hormonal IUDs to regulate cycles and control heavy bleeding. Thyroid medicine may be prescribed if a thyroid disorder is identified. People with anemia from heavy bleeding may receive iron supplements to restore healthy levels. Lifestyle guidance, including changes in diet, stress control, and exercise habits, may also be part of the treatment plan. Follow-up visits help track improvements and adjust treatments as needed so your cycle becomes more stable over time.
FAQs
How do hormones affect menstrual flow and pad usage?
Hormones decide how thick your uterine lining becomes and how quickly it sheds. If your hormones rise or fall sharply, you may see heavier or lighter bleeding. This affects which pad absorbency you need throughout your cycle.
Can a hormonal imbalance cause heavy or irregular bleeding?
Yes. Low progesterone, high estrogen, thyroid issues, or stress can create irregular patterns and heavier cycles.
What type of sanitary towel works best for hormonal skin sensitivity?
Cotton pads, hypoallergenic pads, and breathable options work well for people dealing with irritation triggered by hormonal acne or inflammation.
Can the wrong pad make hormonal symptoms worse?
Pads with harsh materials, fragrances, or poor airflow may irritate when hormones make skin more reactive. Choosing gentler materials often helps.
How often should I change pads if my flow is unpredictable?
If your flow shifts from heavy to light, check your pad every few hours. Many people with unpredictable cycles change pads every 3–4 hours to stay comfortable.
Do hormones affect menstrual odor?
Yes. Hormonal changes can shift vaginal pH, which may make odor stronger. Breathable pads help reduce moisture buildup.
Final Thought
Hormones guide your entire cycle, from flow patterns to PMS intensity. When they shift, your period changes, and so do your sanitary towel needs. Understanding how hormones work helps you choose the right sanitary towel for comfort, absorbency, and skin health. Paying attention to symptoms also gives you a clearer picture of your body’s signals so you know when to adjust your routine or seek medical care. By combining practical period products with healthy habits, you can support more stable cycles and stay comfortable each month.